
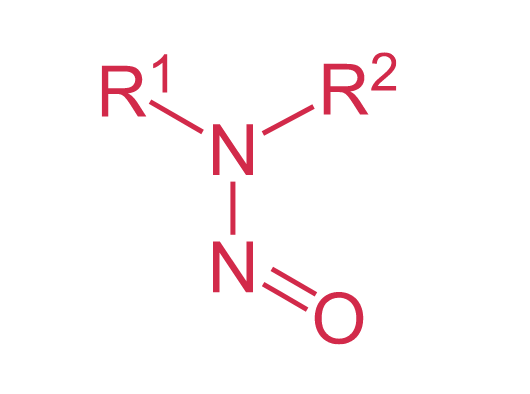
After medicinal products contaminated with nitrosamines had to be recalled just under two years ago, Swissmedic’s own laboratory – the Official Medicines Control Laboratory, or OMCL – developed its own, more sensitive test for detecting contamination. Below we take a closer look at several cases.
The problem of quantity
The tolerated quantity of this genetically harmful substance is always dependent on the maximum daily dose and how long the medicine is used for. For NDMA in valsartan it is 0.3 ppm (parts per million) relative to the quantity of active substance for a lifelong dose of 300 mg daily. As Massimiliano Conti, Head of Swissmedic's laboratory explains, the challenge is therefore to find this tiny amount of contamination. “Swissmedic monitors the medicinal products market. That means that when we test samples, we have to be able to detect and identify the tiniest quantities of nitrosamine and know exactly what we’re looking for at this level.” Impurities are normally subject to limits of 0.1 percent of the active substance (approx. 1,000 ppm); however, this limit is very much lower if the impurity is genetically harmful. When testing for nitrosamines, that means using special analytical methods that are around 3,000 times more sensitive than normal techniques. Or, to take a practical example, when looking for impurities, we are normally looking for something in the order of 1 ml in a litre. In this case we are trying to find that millilitre in 33,000 litres – i.e. something the size of a tanker.New test methods for nitrosamines in sartans
Sartans have antihypertensive and vasodilatory effects, and are used for the treatment of cardiovascular and kidney disease.
